Patient appointments are a bottleneck in the diagnostic pathway of dementia. A diagnosis typically requires several visits, often to different specialists. In addition, only very limited time is allotted for cognitive assessments during patient appointments.
This year’s World Alzheimer Report, created by Alzheimer’s Disease International (ADI), has analysed the “Journey through the diagnosis of dementia”.
One of the key messages from the report is “Globally ageing populations plus diagnostic and treatment breakthroughs will create a tsunami of demand for healthcare systems”.
A series of webinars began to discuss the findings of the report focussing on different aspects. Last week, the focus was on “Diagnosis and health system preparedness”.
Geoff Orry (Person living with dementia and advocate, Scottish Dementia Working Group, UK) shared his experiences of getting a dementia diagnosis which involved visiting three different hospitals.
Dr Soeren Mattke (Research Professor of Economics and the Director of the Center for Improving Chronic Illness Care University of Southern California, USA) presented model predictions which show that wait times will rise before they go down again and concluded that ignoring the problem does not make it go away.
Part of the issue is that there have been very few improvements to diagnostic tools for decades. An example of a method currently used widely by clinicians is the Mini Mental State Examination (MMSE). It consists of a series of questions and tests, examining several different mental abilities, including a person’s memory, attention and language. The MMSE is one of the few tests that translates between clinical trials and standard clinical practice. However, it is a long test that requires a qualified assessor, created in 1975 with very minor modifications to date.
Let’s compare this, for example, to rotary phones which were widely used in 1975. This is not dismissing older methods but contrasting how the phone’s original function to make and receive calls has been tremendously enhanced in modern smartphones. What if we could do something similar and accelerate dementia diagnosis?
Phyllis Ferrell (Global Head, External Engagement, Alzheimer’s and Neurodegeneration, Eli Lilly and Company, USA) pointed out, that science is already moving towards earlier diagnosis, but healthcare systems are not following yet. Patients deserve an early diagnosis not only to take advantage of emerging new treatment options but also to be empowered to make their own decisions.
A study in Brazil presented by Dr Fabiana da Mata (Postdoctoral researcher, Univerisdade Federal De São Paulo, Brazil) found that a lack of recognition of initial symptoms of dementia often leads to a later diagnosis. Regular standardised tests could pick changes up earlier and thus counteract this delay.
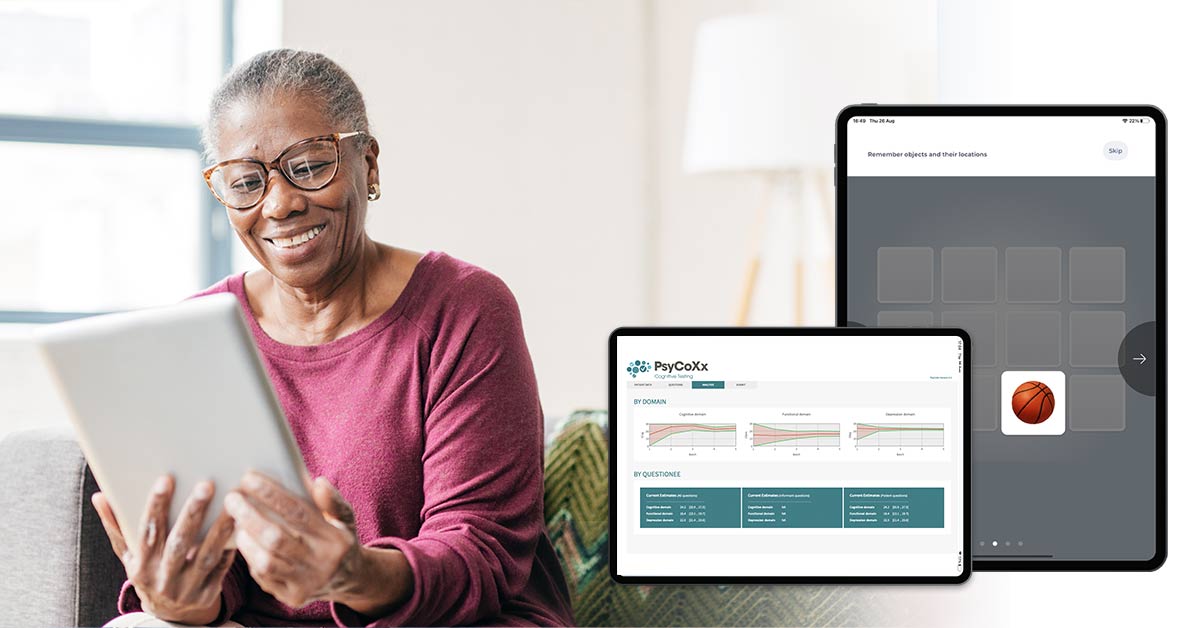
GT Diagnostics, alongside other companies, are working to make fast and reliable assessments available to clinicians by using modern technology. The key aspect here is to ensure new output scores are validated and put into context, for example with a MMSE score, so physicians are provided with an output they can readily interpret since they are familiar with the scale.
The use of technology makes it easier to ensure patients are given different versions of the assessment each time. This way, the learning effect is kept to a minimum. In addition, physicians no longer need to worry about calculating scores as this is done automatically. Physician’s time is thus saved and can be used to look at all the pieces and make a diagnosis based on assessment results and patient history.
The presentation by Prof José A. Morais (Director and Academic Leader of the McGill Dementia Education Program, Canada) identified cultural and language barriers as part of the main barriers in accessing tools to aid diagnosis. He also pointed out that in the global context, the issue of literacy rates should be given more attention.
Tasks that require reading or writing do not work in areas with low literacy rates. Moreover, not all assessments can easily be translated to a different culture. Patient experiences of everyday objects can be very different depending on the patient’s cultural background.
Assessments such as GT Diagnostics’ HiPAL Pro, which is based on images, remove language barriers and thus are accessible to people who cannot read and/or write. Moreover, the use of technology allows a fast and easy adjustment of images to the cultural background.
In areas where most households have access to a computer and/or mobile devices are commonly used, the patient journey could start in the comfort of their own home. Electronic assessments like GT Diagnostics’ HiPAL, which measures memory performance, could link with validated online material such as that provided by ADI to help those, who are worried about their cognitive health to take initial steps at home. Those interested in the topic would then either be reassured that all is well or know they need to contact their physician for help.
The model predictions presented by Dr Soeren Mattke showed that a combination of blood tests and cognitive assessments would improve triage enough to reduce the number of needed appointments below the number of available appointments, which would allow patients to be seen without delay. Combining information from different tests and assessments, ties in with the presentation by Elina Suzuki (Advisor to Director for Employment, Labour and Social Affairs at OECD, France) who reported that data linkage is not good enough and has not improved much since 2018.
We need to work together to accelerate dementia diagnosis, combining results from different tests and providing physicians with a comprehensive view of the different elements.