By Björn Schelter
Diagnosing dementia, or Alzheimer’s disease – its most common form – is a challenging and lengthy process.
The current patient journey is a long and winding road. But why is that the case? Let us look at the diagnostic pathway in more detail.
Initial Suspicion of Cognitive Impairment or Alzheimer’s Disease
It all starts with an initial suspicion that something is wrong with someone’s cognitive abilities – people themselves or their relatives, friends, or colleagues start noticing changes like forgetting names or places. The question arises if this is still normal ageing or already pointing to the first signs of dementia.
Extent of the Problem
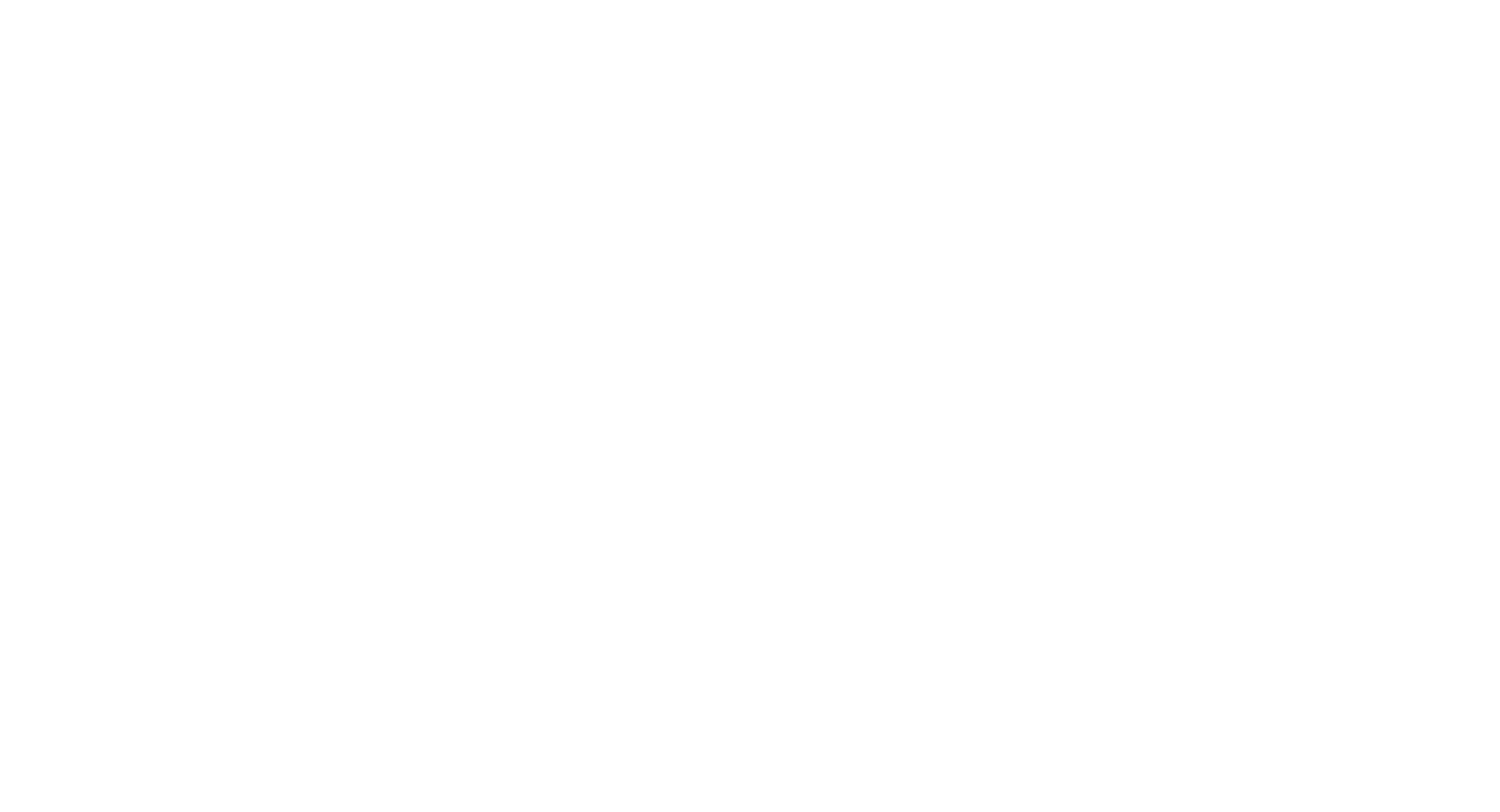
The extent of the problem and the number of cases is depicted by the infographic on the right.
It shows the fraction of people aged 45+ who:
– are diagnosed with dementia in purple
– have the disease but are not diagnosed in blue
– have some form of alteration in their brains that could progress into dementia in orange. Hundreds of millions are potentially impacted.
While we have tools that can be used to aid a diagnosis of dementia, there are far fewer tools that aim to identify the orange group of people who have some level of brain alterations.
This leaves at least two questions: Why are not all people with dementia diagnosed? And how can we identify and support people who are at risk of developing dementia?
ADI Statistics
Alzheimer’s Disease International devoted its World Alzheimer Report 2021 to the challenges faced with a diagnosis. As already depicted in the infographic, it is indeed true, that 75% of people with dementia are not diagnosed. This equates to 41 million people. Again, raising the question, why are they not diagnosed?
Don’t we have the right tools? Are our healthcare systems not fit for purpose to identify these people or maybe the problem is that 33% of clinicians do believe that nothing can be done about dementia? So why bother with a diagnosis? And how much does the long and winding diagnostic journey contribute to all of this?
Diagnostics is an expert business, not a primary care one; time pressure and pay per visit models for primary care doctors are counterproductive to a complex and sensitive dementia diagnosis.
Currently, it is not possible to go from early suspicion of symptoms to a diagnosis in a primary care setting. The more experts need to be involved, the longer and more difficult the process will become.
The Long and Winding Road
What happens after initial suspicion of symptoms?

People affected might seek help from primary care physicians. Having only limited time for an appointment (typically follow up appointments are needed), getting initial tests done, ruling out some other explanations for cognitive impairment, ultimately sending the person on the long and winding road.
Typically, when a specialist referral is needed, there is usually a long waiting period. During the appointments, there are more tests, again, including tests that rule out other reasons for the impairment. These specialised tests often rely on the technology of the last century; paper-based tests developed when we were still using rotary phones. If the initial suspicion is confirmed, referral to specialised imaging centres is often the next step, blood tests, and other tests including cerebrospinal fluid tests to ultimately support the initial suspicion of an Alzheimer’s disease diagnosis.
Once the diagnosis is made, often only 6 months after the first appointment with the primary care physician, the next steps are discussed.
While new treatment options come to the market, the standard is still symptomatic treatments, treatments that give a short-term boost but do not ultimately alter the course of the disease. For most people, management of symptoms is their only option. Ultimately, the outcome is often long-term care.
Six months going through a process to reach a diagnosis, people with Alzheimer’s disease then face limited treatment options and long-term care as their future. This is what we are currently looking at.
It is very important to change the whole patient journey and to give dementia diagnostics a completely different future.
Future of Diagnostics
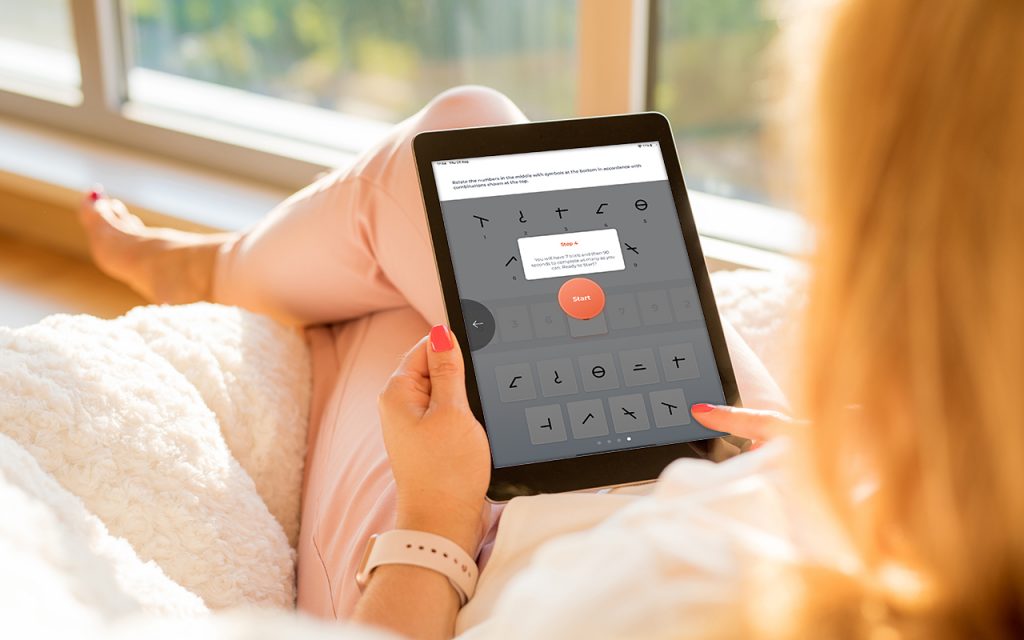
The key step is to bring Alzheimer’s disease diagnostics into the 21st century. We do not use rotary phones anymore, why would we still use technology from the same decade to diagnose such a devastating disease? We need to bring dementia diagnosis into the 21st century, the age of powerful mobile technology and artificial intelligence.
And I mean that quite literally, we should start using mobile phones and tablets together with artificial intelligence to support a diagnosis of dementia.
What Could a Patient Journey Look Like?

So what can a patient journey look like in the future when we use such modern technology? People will start their journey in the comfort of their homes, and rely on intuitive and engaging tools to see if something might be of concern.
Initial Appointment
If there is a reason for concern, the next steps will lead them to a much more efficient route. In the waiting room of the primary care provider, advanced self-administered diagnostics can be used to maximise time during the initial consultation with the primary care physician.
Through a more effective initial screening at earlier stages of the disease, either a diagnosis can be reached at this point or, if a referral to a specialist is needed, the streamlined process will allow reaching a diagnosis more efficiently. Test results can be exchanged very efficiently between primary care physicians and neurologists or old age psychiatrists through modern technology.
Treatment Prescribed
With new safe and disease-modifying treatments coming to the market, people with Alzheimer’s disease can be put on the path to a brighter future very efficiently. The diagnostic tools then become monitoring tools to capture the effectiveness of the treatment.
Outcome
This obviously translates into a much better quality of life for much longer. People with Alzheimer’s disease will be able to live independently for much longer, and they can enjoy all their day to day activities.